Open-Angle Glaucoma Sufferer's FAQ
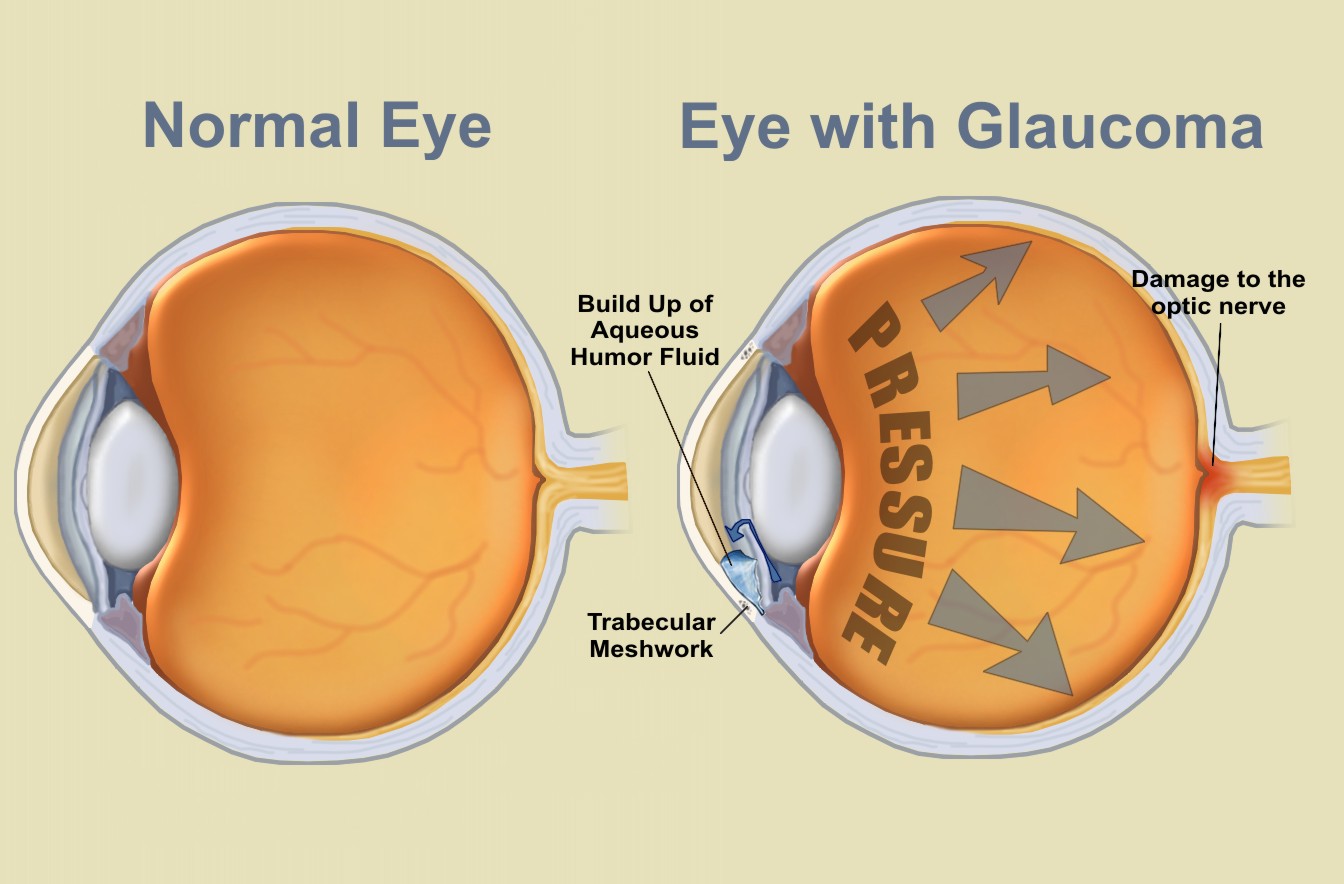
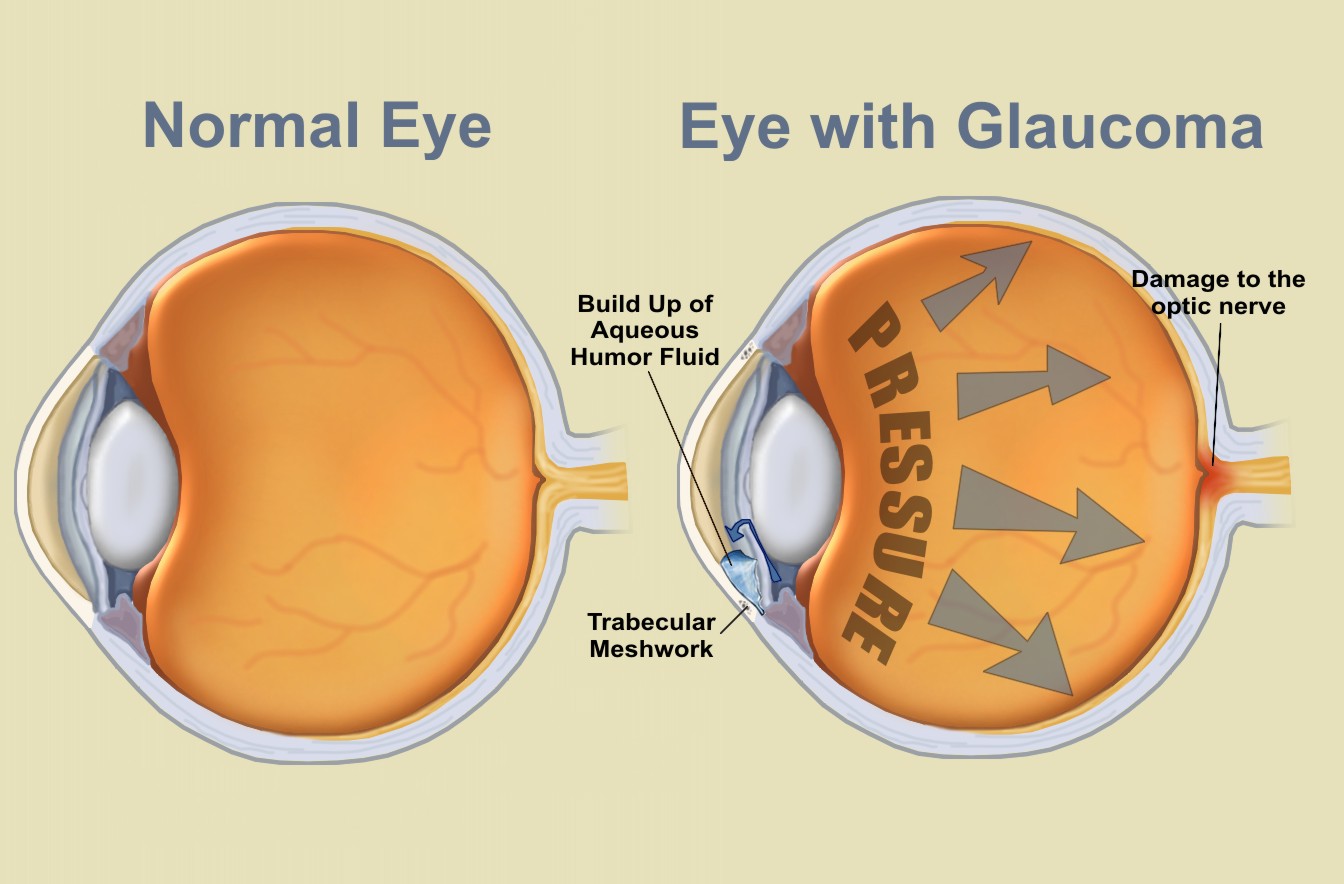
Glaucoma—cause
- High Intraocular Pressure (IOP).
- Intraocular pressure (IOP)
is the fluid pressure inside the eye.
Tonometry
 is the method
eye care professionals use to determine this. IOP is an important
aspect in the evaluation of patients at risk from
glaucoma.
Most tonometers are calibrated to measure pressure in millimeters of
mercury (mmHg).
The increased pressure prevents the blood flow to the optic nerve
and the cells near the periphery die and the damage gradually moves inward.
Because it occurs over a long period, you don't notice the loss
until it is too late. Your brain fills in details that simply aren't
there which makes your life very dangerous. Especially when you
drive.
is the method
eye care professionals use to determine this. IOP is an important
aspect in the evaluation of patients at risk from
glaucoma.
Most tonometers are calibrated to measure pressure in millimeters of
mercury (mmHg).
The increased pressure prevents the blood flow to the optic nerve
and the cells near the periphery die and the damage gradually moves inward.
Because it occurs over a long period, you don't notice the loss
until it is too late. Your brain fills in details that simply aren't
there which makes your life very dangerous. Especially when you
drive.
- Hereditary.
- My mother suffers from the exact same issues with approximately
the same losses in each eye (80% in the
left and
60% in the
right eye). I believe her mother also suffered from the disease
although I don't think she knew it. This suggests to me the disease
may be due to a defective
gene on one of the X-chromosomes and thus carried down the female
line. This also explains why one sibling gets glaucoma whereas another
does not since they received the other of the pair of X-chromosomes
from their mother. Neither my brother nor my sister have any symptoms.
- Why is it so hard to discover?
- It is estimated there are 4 million people, in the USA alone,
with glaucoma—mostly with Primary Open-Angle Glaucoma (POAG)—only
50% have been diagnosed. The disease is invariably discovered long after the damage is done.
 Individuals
predisposed to glaucoma should be identified at the earliest possible
stages of the disease, so that treatment can be initiated before the
optic nerve is irreversibly damaged. Although current therapy is not
curative, for many patients lowering the IOP using currently available
pharmaceutical and/or surgical approaches can slow the progression of
the disease and limit the overall loss of vision. Thus, biomarkers might
be invaluable tools to identify individuals at risk for disease and,
depending on the approach, could serve to measure the outcomes of therapies.
Individuals
predisposed to glaucoma should be identified at the earliest possible
stages of the disease, so that treatment can be initiated before the
optic nerve is irreversibly damaged. Although current therapy is not
curative, for many patients lowering the IOP using currently available
pharmaceutical and/or surgical approaches can slow the progression of
the disease and limit the overall loss of vision. Thus, biomarkers might
be invaluable tools to identify individuals at risk for disease and,
depending on the approach, could serve to measure the outcomes of therapies.
- Symptoms that sent me to the doctor.
- I kept banging my elbows on door jambs and falling over or kicking
things on the floor. By the time it was diagnosed, it was already too
late. There were other symptoms that I had attributed to seasonal allergies.
- Is there a test that I can perform at home?
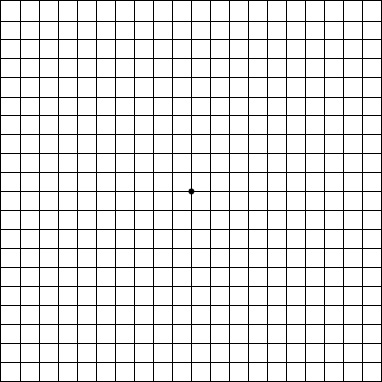 Yes, a very simple one that only takes a few seconds. It's called an Amsler Grid.
Get the full-size version and hold it 12-14 inches away from your eyes. Cover one eye, then focus on the dot in the center. Can you see all corners and sides of the grid? Don't forget to test both eyes. My
left eye is considerably worse than my right.
If you have a telescope, you will notice that you can’t see the whole image through the lens and likely it will be worse with one eye than the other. Spot lights and lasers such as car brake lights
will have refractive patterns or haloes around them. Distant objects
such as the moon and stars may appear doubled. You may suffer uncontrollable
panic attacks as your brain becomes confused—if this happens, close
your eyes and hold on to something until the feeling goes away. Avoid
large areas that are predominantly lit by fluorescent lighting such
as stores. The
Gears Illusion looks like it is standing still if you have
Glaucoma.
Yes, a very simple one that only takes a few seconds. It's called an Amsler Grid.
Get the full-size version and hold it 12-14 inches away from your eyes. Cover one eye, then focus on the dot in the center. Can you see all corners and sides of the grid? Don't forget to test both eyes. My
left eye is considerably worse than my right.
If you have a telescope, you will notice that you can’t see the whole image through the lens and likely it will be worse with one eye than the other. Spot lights and lasers such as car brake lights
will have refractive patterns or haloes around them. Distant objects
such as the moon and stars may appear doubled. You may suffer uncontrollable
panic attacks as your brain becomes confused—if this happens, close
your eyes and hold on to something until the feeling goes away. Avoid
large areas that are predominantly lit by fluorescent lighting such
as stores. The
Gears Illusion looks like it is standing still if you have
Glaucoma.
How it affects you
- If you lead an active life, the effect will be devastating.
- Up until my diagnosis in 2006 I led a very active life. Skiing,
motorcycle racing, hiking, and lots of other outdoor activities. I have
two children at school and can now no longer do the things I enjoy because
of the risk of injury that would prevent me from working.
- Can you drive?
- Possibly, if you are aware of your limitations and adjust accordingly.
Scan left and right continuously as you drive (it will soon become
second nature). Choose your trips carefully,
avoid traffic, make use of freeways (less traffic coming in from the
side), and try not to change lanes. Check at least twice before pulling
out and wait if you are not sure. Look at the gap between your vehicle
and others around you as you cannot rely on your 3D vision, especially
as you come to a stop behind the car in front. Always travel by the
same route if possible. Avoid travelling in unfamiliar places. Let others
drive if you are not alone. Give yourself plenty of time to make maneuvers
and always check vehicles close by. Select a vehicle which will help
such as the
Mercedes ML320 which has sensors all around for people and
vehicles and also has adaptive distance control for cruising. Do NOT
drive at night except in an emergency.
The Association between Primary Open-Angle Glaucoma
and Motor Vehicle Collisions is statistically significant.
- Environment.
- You may suffer uncontrollable panic attacks as your brain becomes
confused—if this happens, close your eyes and hold on to something
until the feeling goes away. Avoid large areas that are predominantly
lit by fluorescent lighting such as stores. About the longest I can
stand being in a store is thirty minutes and it starts getting uncomfortable
after ten minutes.
- Drooping eyelid.
- The medical term for drooping or droopy eyelid is Ptosis or Blepharoptosis.
In severe cases of glaucoma the brain doesn’t bother opening the eye
fully. This is particularly noticeable on photographs.
Is there a cure?
- No, it is a permanent loss.
-
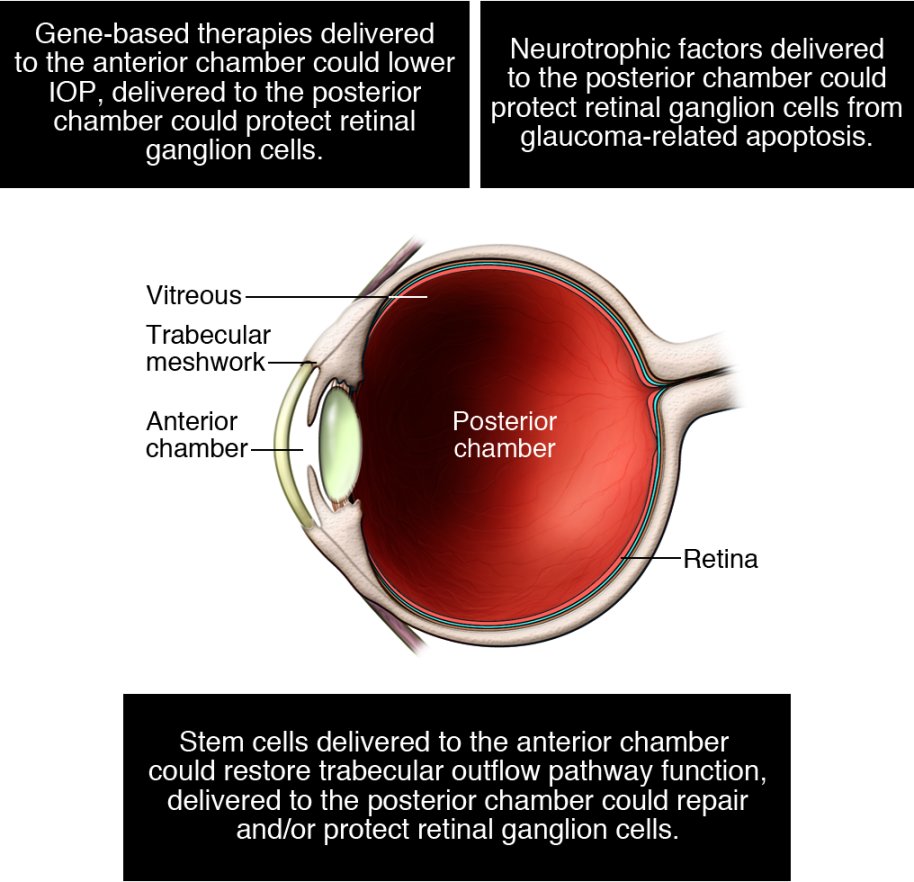
 When
I was 46 I started having reading problems. Up until then my
eyesight was perfect. At the time it was recommended that I see an
eye specialist as I was showing signs of vision loss. I started
wearing glasses for reading but did not heed the advice to see a
specialist. In 2006, at the age of 58, I was diagnosed with
glaucoma. Realizing that I could have done something to save my
sight all those years ago, was a blow I have not been able to come
to grips with to this day. Operations
such as
Trabeculectomy can only prevent further damage. But there
is hope with
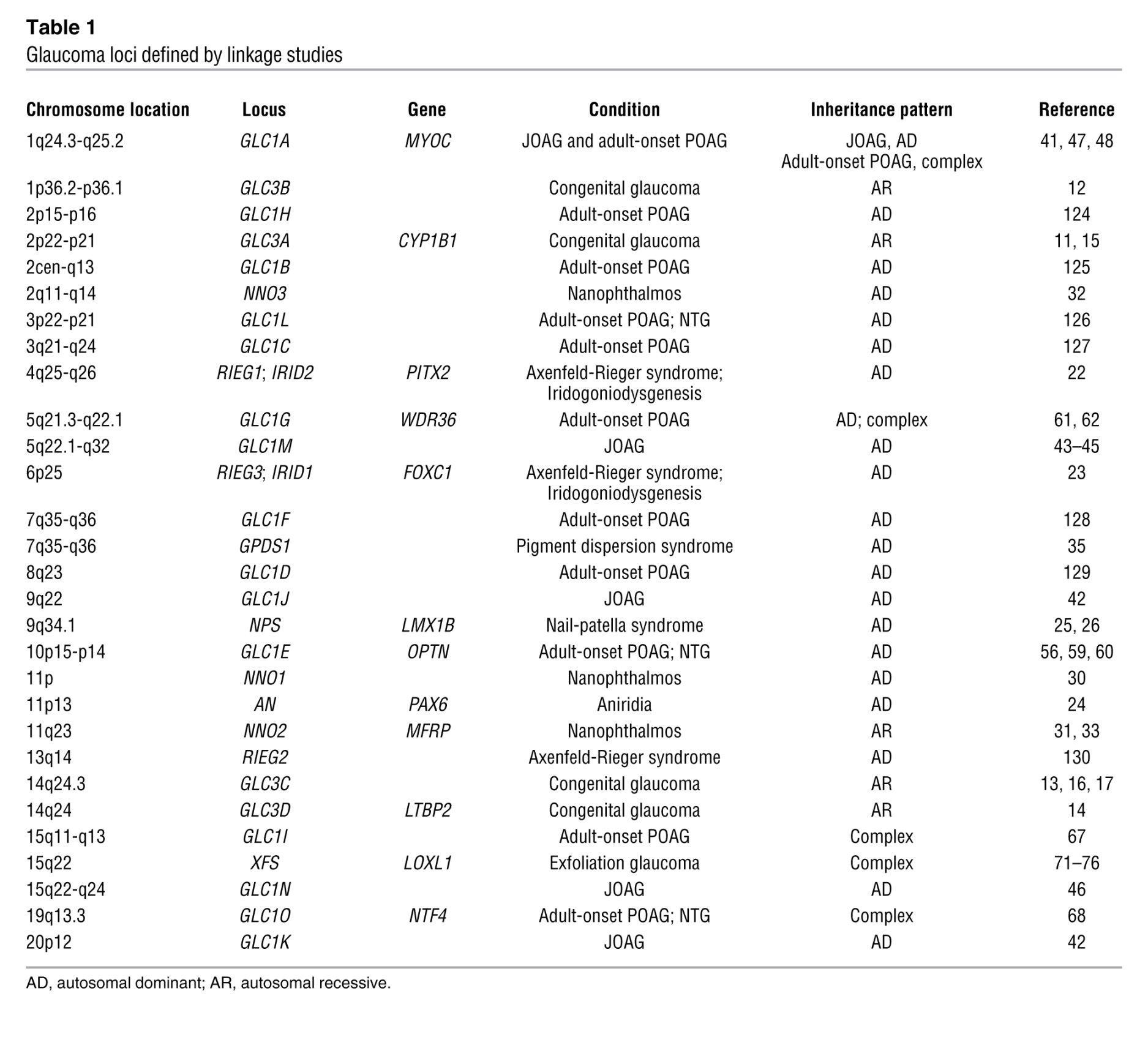
upcoming stem cell research. Identifying the
genes (and
here) involved
in glaucoma will go a long way to finding the cure. See the research
funded by the
Glaucoma Research Foundation
When
I was 46 I started having reading problems. Up until then my
eyesight was perfect. At the time it was recommended that I see an
eye specialist as I was showing signs of vision loss. I started
wearing glasses for reading but did not heed the advice to see a
specialist. In 2006, at the age of 58, I was diagnosed with
glaucoma. Realizing that I could have done something to save my
sight all those years ago, was a blow I have not been able to come
to grips with to this day. Operations
such as
Trabeculectomy can only prevent further damage. But there
is hope with
upcoming stem cell research. Identifying the
genes (and
here) involved
in glaucoma will go a long way to finding the cure. See the research
funded by the
Glaucoma Research Foundation
- Types of eye drops.
-
 Here is a tip for those having difficulty using eye drops. Because I couldn't see the bottle, I found myself jamming eyelashes into my eye, missing my eye completely, and so on. So, I came up with a foolproof method of applying the drops. If you are right-handed, place the eye-drop
bottle on the back of your index finger while lining up the top of the bottle with the tip of your finger. Now, pull open your lower eyelid with your index finger and apply the eye drops by squeezing the bottle with your left hand. The bottle is perfectly lined up even though you can't see it.
Here is a tip for those having difficulty using eye drops. Because I couldn't see the bottle, I found myself jamming eyelashes into my eye, missing my eye completely, and so on. So, I came up with a foolproof method of applying the drops. If you are right-handed, place the eye-drop
bottle on the back of your index finger while lining up the top of the bottle with the tip of your finger. Now, pull open your lower eyelid with your index finger and apply the eye drops by squeezing the bottle with your left hand. The bottle is perfectly lined up even though you can't see it.

-
Alpha agonists work to both decrease production of fluid and
increase drainage.
-
Beta blockers work by decreasing production of intraocular
fluid.
-
Carbonic anhydrase inhibitors (CAIs) reduce eye pressure
by decreasing the production of intraocular fluid. These are available
as eye drops and as pills.
-
Combined medications can offer an alternative for patients
who need more than one type of medication.
-
Prostaglandin analogs work by increasing the outflow of
intraocular fluid from the eye. They have few systemic side effects
but are associated with changes to the eye itself, including change
in iris color and growth of eyelashes.
- Cosopt.
- Dorzolamide hydrochloride-timolol maleate ophthalmic solution (0.2%/0.05%), formerly
marketed as
Cosopt by Merck is now generic. I had to stop using this as it caused
severe stinging after a few months of use. After switching to another
medication the stinging slowly went away. I recently switched to the
newer Cosopt PF (Preservative Free) which, to date, has showed no
signs of the stinging that the regular Cosopt did. The generic
Dorzolamide-Timolol Maleate (22.3mg/6.8mg per ml) is also not a problem for me. WARNING: Make sure your doctor prescribes this as Dorzolamide-Timolol (22.3mg/6.8mg per ml) and
NOT 0.2%/0.05% or you will be charged for the expensive Tier 4 drug.
- Combigan.
- Brimonidine tartrate/timolol maleate ophthalmic solution 0.2%/0.5%
is sold as
Combigan.
- Xalatan.
- Latanoprost 0.005%. This is now generic.
- Travatan.
- Travaprost 0.004%. This is made from some of the most valuable material
on the planet. As a 0.004% solution and ~$90 for a 2.5ml bottle then
this works out at ~$535,000/gram.
- Timolol.
- Timolol Maleate 0.5%. This is generic.
 is the method
eye care professionals use to determine this. IOP is an important
aspect in the evaluation of patients at risk from
glaucoma.
Most tonometers are calibrated to measure pressure in millimeters of
mercury (mmHg).
The increased pressure prevents the blood flow to the optic nerve
and the cells near the periphery die and the damage gradually moves inward.
Because it occurs over a long period, you don't notice the loss
until it is too late. Your brain fills in details that simply aren't
there which makes your life very dangerous. Especially when you
drive.
is the method
eye care professionals use to determine this. IOP is an important
aspect in the evaluation of patients at risk from
glaucoma.
Most tonometers are calibrated to measure pressure in millimeters of
mercury (mmHg).
The increased pressure prevents the blood flow to the optic nerve
and the cells near the periphery die and the damage gradually moves inward.
Because it occurs over a long period, you don't notice the loss
until it is too late. Your brain fills in details that simply aren't
there which makes your life very dangerous. Especially when you
drive.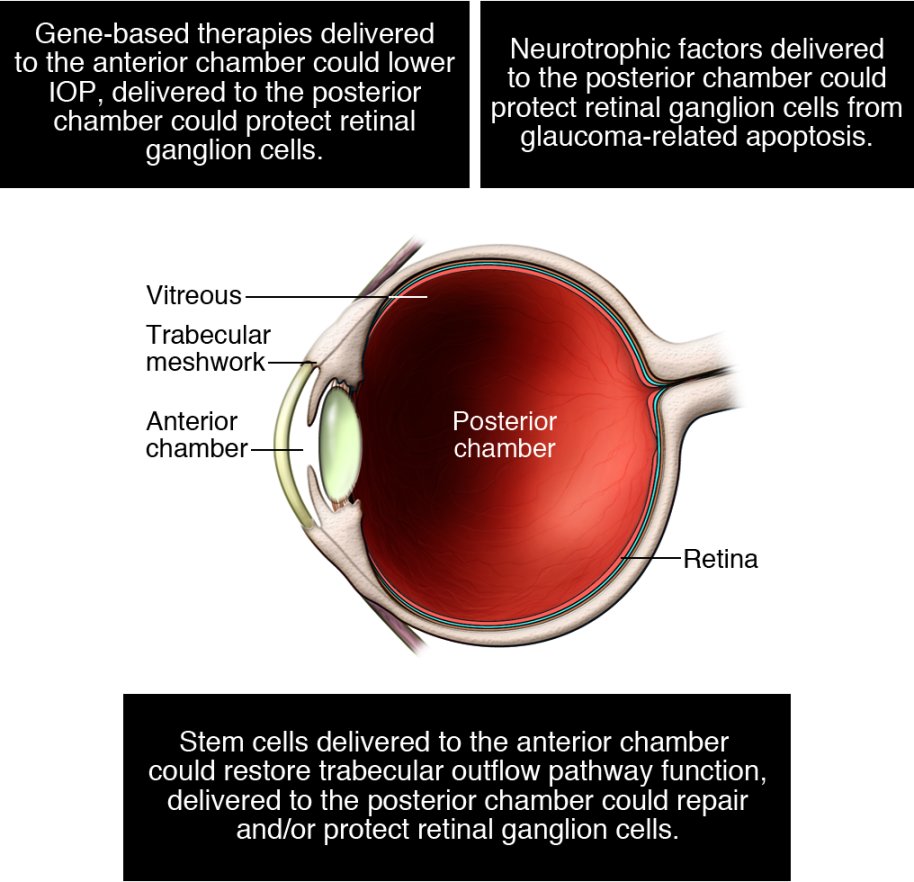 Individuals
predisposed to glaucoma should be identified at the earliest possible
stages of the disease, so that treatment can be initiated before the
optic nerve is irreversibly damaged. Although current therapy is not
curative, for many patients lowering the IOP using currently available
pharmaceutical and/or surgical approaches can slow the progression of
the disease and limit the overall loss of vision. Thus, biomarkers might
be invaluable tools to identify individuals at risk for disease and,
depending on the approach, could serve to measure the outcomes of therapies.
Individuals
predisposed to glaucoma should be identified at the earliest possible
stages of the disease, so that treatment can be initiated before the
optic nerve is irreversibly damaged. Although current therapy is not
curative, for many patients lowering the IOP using currently available
pharmaceutical and/or surgical approaches can slow the progression of
the disease and limit the overall loss of vision. Thus, biomarkers might
be invaluable tools to identify individuals at risk for disease and,
depending on the approach, could serve to measure the outcomes of therapies.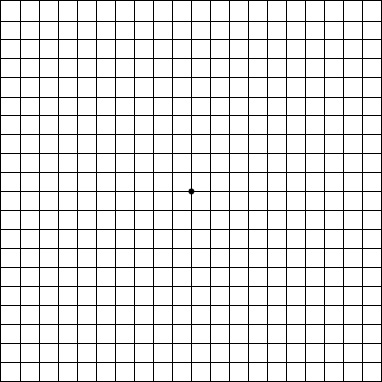 Yes, a very simple one that only takes a few seconds. It's called an Amsler Grid.
Get the full-size version and hold it 12-14 inches away from your eyes. Cover one eye, then focus on the dot in the center. Can you see all corners and sides of the grid? Don't forget to test both eyes. My
left eye is considerably worse than my right.
If you have a telescope, you will notice that you can’t see the whole image through the lens and likely it will be worse with one eye than the other. Spot lights and lasers such as car brake lights
will have refractive patterns or haloes around them. Distant objects
such as the moon and stars may appear doubled. You may suffer uncontrollable
panic attacks as your brain becomes confused—if this happens, close
your eyes and hold on to something until the feeling goes away. Avoid
large areas that are predominantly lit by fluorescent lighting such
as stores. The
Gears Illusion looks like it is standing still if you have
Glaucoma.
Yes, a very simple one that only takes a few seconds. It's called an Amsler Grid.
Get the full-size version and hold it 12-14 inches away from your eyes. Cover one eye, then focus on the dot in the center. Can you see all corners and sides of the grid? Don't forget to test both eyes. My
left eye is considerably worse than my right.
If you have a telescope, you will notice that you can’t see the whole image through the lens and likely it will be worse with one eye than the other. Spot lights and lasers such as car brake lights
will have refractive patterns or haloes around them. Distant objects
such as the moon and stars may appear doubled. You may suffer uncontrollable
panic attacks as your brain becomes confused—if this happens, close
your eyes and hold on to something until the feeling goes away. Avoid
large areas that are predominantly lit by fluorescent lighting such
as stores. The
Gears Illusion looks like it is standing still if you have
Glaucoma.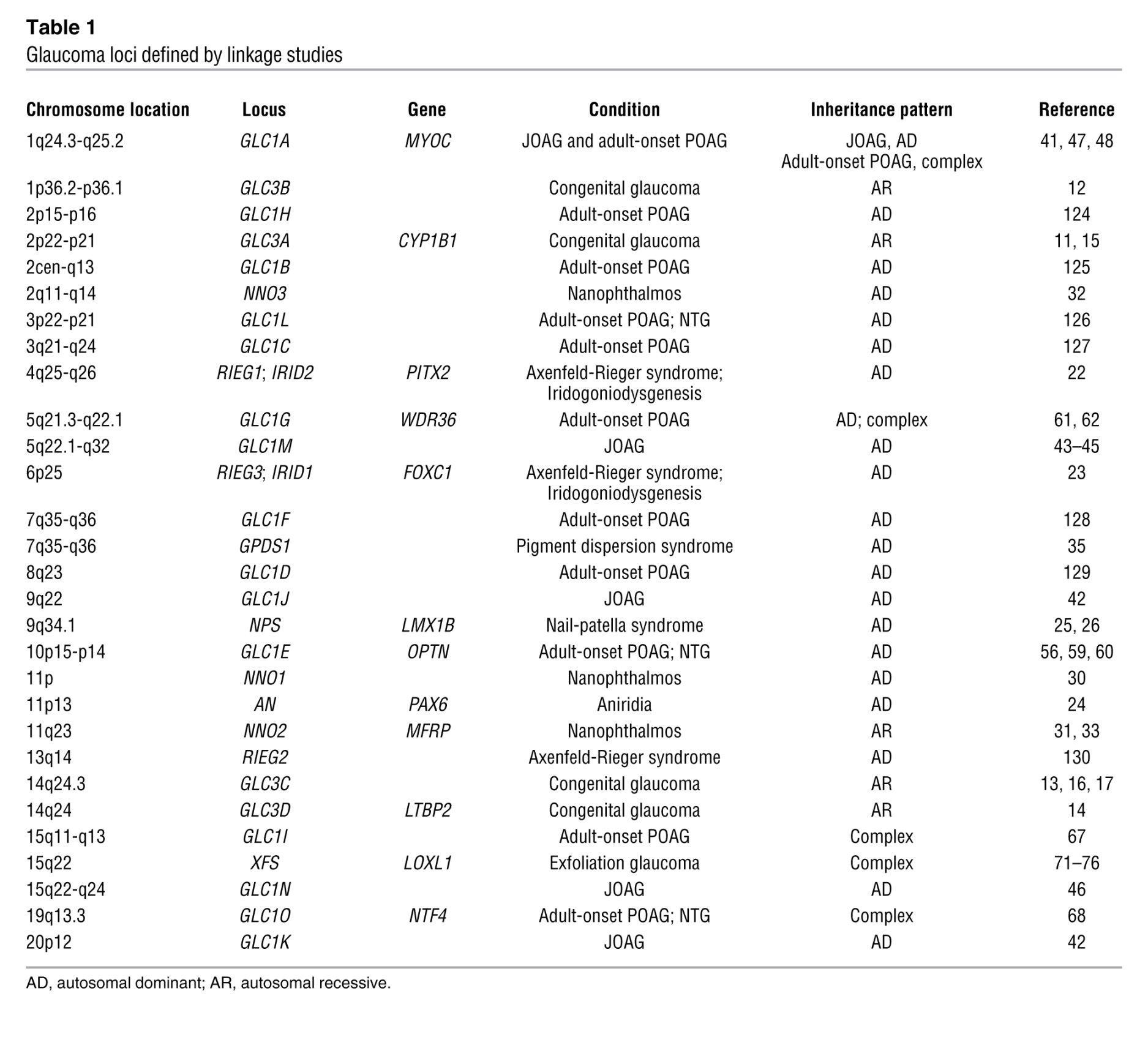 When
I was 46 I started having reading problems. Up until then my
eyesight was perfect. At the time it was recommended that I see an
eye specialist as I was showing signs of vision loss. I started
wearing glasses for reading but did not heed the advice to see a
specialist. In 2006, at the age of 58, I was diagnosed with
glaucoma. Realizing that I could have done something to save my
sight all those years ago, was a blow I have not been able to come
to grips with to this day. Operations
such as
Trabeculectomy can only prevent further damage. But there
is hope with
upcoming stem cell research. Identifying the
genes (and
here) involved
in glaucoma will go a long way to finding the cure. See the research
funded by the
Glaucoma Research Foundation
When
I was 46 I started having reading problems. Up until then my
eyesight was perfect. At the time it was recommended that I see an
eye specialist as I was showing signs of vision loss. I started
wearing glasses for reading but did not heed the advice to see a
specialist. In 2006, at the age of 58, I was diagnosed with
glaucoma. Realizing that I could have done something to save my
sight all those years ago, was a blow I have not been able to come
to grips with to this day. Operations
such as
Trabeculectomy can only prevent further damage. But there
is hope with
upcoming stem cell research. Identifying the
genes (and
here) involved
in glaucoma will go a long way to finding the cure. See the research
funded by the
Glaucoma Research Foundation Here is a tip for those having difficulty using eye drops. Because I couldn't see the bottle, I found myself jamming eyelashes into my eye, missing my eye completely, and so on. So, I came up with a foolproof method of applying the drops. If you are right-handed, place the eye-drop
bottle on the back of your index finger while lining up the top of the bottle with the tip of your finger. Now, pull open your lower eyelid with your index finger and apply the eye drops by squeezing the bottle with your left hand. The bottle is perfectly lined up even though you can't see it.
Here is a tip for those having difficulty using eye drops. Because I couldn't see the bottle, I found myself jamming eyelashes into my eye, missing my eye completely, and so on. So, I came up with a foolproof method of applying the drops. If you are right-handed, place the eye-drop
bottle on the back of your index finger while lining up the top of the bottle with the tip of your finger. Now, pull open your lower eyelid with your index finger and apply the eye drops by squeezing the bottle with your left hand. The bottle is perfectly lined up even though you can't see it.
